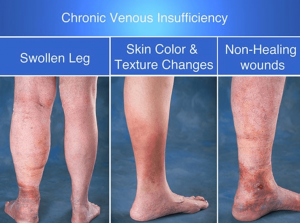
Discolored Skin? You May Have Chronic Venous Insufficiency
Are you beginning to notice discolored skin your legs with no known cause? The cause may be chronic venous insufficiency.
What is chronic venous insufficiency?
The veins in your legs are very sensitive, but also vitally important to a well-functioning body. They’re not only important to circulation in your legs themselves, but they also are responsible for bringing blood to your heart. The veins in your legs have a valve that ensure that the blood in your leg only flows one way, due to their relationship with your heart. When you have chronic venous insufficiency, the valves that control the direction that the blood in your legs flow aren’t working correctly. When the valves in the veins in your legs don’t work correctly, it causes blood to pool, collect, or in some cases even clot, in the vein.
In layman’s terms, chronic venous insufficiency is when the veins in your legs are malfunctioning and making it difficult for the blood to flow back to your heart. One way of thinking of it is like a “traffic jam” in your veins, the blood will flow, but slowly, and it’s likely to pool in one place. The worst case scenario is that this causes a blood clot, which can be fatal. It’s easy to see how this can easily cause discoloration.
Chronic venous insufficiency isn’t a rare condition—it’s extremely common. If you think you may have chronic venous insufficiency, keep your eyes open for some of the first red flags: pain and heaviness in the affected leg. It’s not a regular pain, like you might experience from a bruise or other injury. Many people who’ve suffered with chronic venous insufficiency have described the leg pain associated with it as pulsating throughout the whole limb.
Chronic venous insufficiency can lead to blood clots, but it also can be caused by blood clots that damage the valves in the affected leg. This eventually leads to venous hypertension and edema (also called swelling), as well as a range of other complications. Chronic venous insufficiency isn’t a cut and dry diagnosis, there are three different stages of the disease. Depending on what stage you’re in, this will determine the care you need to receive.
The stage of chronic venous insufficiency are:
STAGE 1:
Swelling and discoloration.
STAGE 2:
Swelling, discoloration, and dermatitis.
STAGE 3:
Varicose veins, swelling, discoloration, dermatitis and ulceration
Needless to say, chronic venous insufficiency is a condition you will want to seek immediate treatment from Cardio Vascular Specialists for. If left untreated, the following may occur: pain, further swelling, cramping in the affected leg or legs, extreme skin discoloration or changes, deep varicose veins, and leg ulcers. While in most cases, chronic venous insufficiency doesn’t pose a serious health risk, it can lead to conditions that can be fatal. In addition to this, it can also lead to disabling pain, that may prevent you from leading a normal life.
Risk factors
There are certain risk factors that make developing chronic venous insufficiency more likely. They include, but aren’t limited to: being overweight, pregnancy, a family history of chronic venous insufficiency, a leg injury, a leg surgery, a history of blood clots, high blood pressure in the leg veins overtime (usually due to sitting or standing for extended periods of time), a long term lack of exercise, smoking, certain medications like birth control, a blood clot deep in the vein (typically in the calf or thigh, this is called deep vein thrombosis), and swelling close to the vein due to an allergic reaction. These aren’t the only causes and risk factors, however, so even if these situations seem unfamiliar to your lifestyle or circumstances, you may still be experiencing chronic venous insufficiency.
It’s essential to always double check with a license physician to ensure a correct diagnosis.
What are the symptoms of chronic venous insufficiency?
If you feel like you may have chronic venous insufficiency, there are a number of symptoms you can look out for. The symptoms of chronic venous insufficiency include, but aren’t limited to: swelling in your legs, swelling in your ankles, tightness in your calves or other parts of your legs, painful legs or ankles, pain that stops or gets better with rest, pain that increases with exercise, discolored skin (usually of a brown color) near the ankles, varicose veins, leg ulcers that resist treatment, restless leg syndrome, cramping in your legs or ankles, and muscle spasms.
These symptoms may occur together or in isolation. They may also mimic other health conditions. If these symptoms seem familiar to your situation, please talk to your healthcare provider. They will be able to do the requisite tests to ensure you get the correct diagnosis.
Getting a diagnosis for chronic venous insufficiency
A licensed physician or healthcare provider will review your medical history. Next, they will typically give you an exam. In getting a diagnosis for chronic venous insufficiency, a common next step is a duplex ultrasound. A duplex ultrasound looks at the blood flow and the infrastructure of the veins in your legs. When the ultrasound checks the blood flow, it will look at the direction and speed of the blood flow. All of these factors can help your licensed physician determine if you have chronic venous insufficiency.
 Getting treatment for chronic venous insufficiency
Getting treatment for chronic venous insufficiency
Chronic venous insufficiency often causes swelling, due to the decreased oxygen to your legs. One way to treat this is external compression, such as with compression stockings. Pneumatic compression devices have also been known to help chronic venous insufficiency. Pumping is another method that works.
To determine a workable treatment plan, your licensed physician will consider the following factors: your age, your overall health, your medical history, how serious your symptoms are, your history with certain medicines, allergies, your experience with other treatments and therapies, if your physician expects your condition to worsen, your lifestyle, and your comfort level with various treatment plans.
Your treatment plan may look many different ways. Here are some potential ways your treatment plan may look for your chronic venous insufficiency:
Keeping your legs elevated to reduce swelling and increase blood flow, wearing compression stockings in the evening or during the day, regular exercise to improve your blood flow, medicines that increase blood flow, medicines that heal leg ulcers, aspirin which can be used for blood flow or to help heal leg ulcers, medicines that are used to draw fluid from the body such as diuretics (these are not often used due to how hard they are on the kidneys), endogenous laser ablation or radio frequency ablation which puts a tube that provides heat to the affected area to increase your blood flow, or sclerotherapy (a chemical that’s injected into your veins that causes scarring so other veins can become stronger and carry blood to the hearty).
Your doctor may also recommend surgery. Surgery is only recommended in the most severe cases of chronic venous insufficiency. Usually, when surgical intervention happens, it’s ligation, however, other routes are certainly an option as well. During a ligation surgery for chronic venous insufficiency, the vein in question is tied so there’s no more blood flow. In the event that the vein is heavily damaged, the vein will be removed all together. When the vein is removed all together, it’s no longer ligation surgery. This type of procedure is called vein stripping.
Three other options that may be on the table in severe cases of chronic venous insufficiency are vein repair, vein bypass, and vein transplants. During a vein repair, the vein or the valves are fixed. Typically, this is done with a catheter. In a vein transplant, your vein or valve will be replaced with a healthy vein from somewhere else in your body. Finally, a vein bypass is when your doctor takes another vein to reroute blood around your affected vein. This is only done in extremely severe cases of chronic venous insufficiency, and require lengthy hospital stays.
Outside of the extreme cases described above, this is typically what a treatment plan will look like for patients in the different stages of chronic venous insufficiency.
Patients with stage one chronic venous insufficiency
Patients in stage one chronic venous insufficiency will be advised to wear elastic compression stockings and also be educated on proper skin care to prevent further swelling or skin discoloration.
Patients with stage one chronic venous insufficiency will be advised the most conservatively. Treatment starts with compression stockings. You can find compression stockings at most pharmacies and department stores. They come in a variety of styles: below-the-knee, above-the-knee, and pantyhose. These days they are also fun and fashionable, so wearing them doesn’t have to be a pain. More importantly than how they look or what style they come in, they come in a range of different compressions. The compressions start at 8 mm Hg and go up to 50 mm Hg. When choosing the right compression stocking, make sure you talk to your doctor. Your doctor will advise you of which compression stocking makes the most sense for your treatment plan. In some areas, if you are looking for compression stockings with a compression of more than 20 mm Hg, you will need a prescription.
Compression stockings have some measure of risk, even though they are a conservative option. Always make sure you take your compression stockings off. Also be sure to wash and properly dry them. The next step is to do the same for your skin! Make sure you are regularly and properly moisturizing. Chronic venous insufficiency can cause your skin to crack. If your skin isn’t ulcerated or swollen, your doctor may recommend you use an anti-itch cream, such as hydrocortisone. Zinc oxide can be used to protect the skin. You may also use an anti-fungal cream as a preventive to protect the skin in the compression stocking.
In the event your skin is leaking any fluids, doctors will advise you to use a wet compress. If the leaking or wound has become an ulcer, your doctor will advise you of how to take care of it to maintain blood flow. In either of these two situations, also make sure that it’s safe to use your compression stocking.
If your compression stockings don’t have the right fit or aren’t properly cleaned, they can make your chronic venous insufficiency worse. The wrong compression stockings make your chronic venous insufficiency worse by blocking blood flow. There’s evidence that suggests that compression stockings and certain prescription medications are extremely effective for chronic venous insufficiency.
Patients with stage two chronic venous insufficiency
Patients with stage two chronic venous insufficiency will be advised to wear compression stockings as well. They will also be educated on how to properly care for their skin, as described above. They are more likely to be prescribed lotions and steroids for any skin conditions. At stage two, it’s encouraged to get a surgical consultation.
Patients with stage three chronic venous insufficiency
Patients with stage three chronic venous insufficiency will wear compression stockings. They also will be armed with a good preventative regimen for ulcers. Preventative treatment for ulcers includes antiseptic solution, and bio-occlusive dressings. This is also when doctors will recommend pneumatic therapy. Surgical consultation is strongly recommended.
What you need to know about surgery for chronic venous insufficiency
Less than 10% of people suffering with chronic venous insufficiency end up getting surgical treatment. Your doctor will recommend an appropriate treatment for you.
Preventing chronic venous insufficiency
Prevention is always easier than maintenance and chronic venous insufficiency is no exception. If you want to reduce your risk, here are some steps you can take to prevent chronic venous insufficiency: ensure you’re getting proper vitamins, eat a balanced diet, quit smoking and excessive drinking, create a daily exercise plan, don’t wear tight girdles or belts, stay at a healthy weight, and avoid prolonged sitting and standing. Interestingly, both sitting and standing put people at risk. There’s a myth that prolonged standing may help you prevent chronic venous insufficiency. In fact, it’s just as dangerous as sitting for long periods of time!