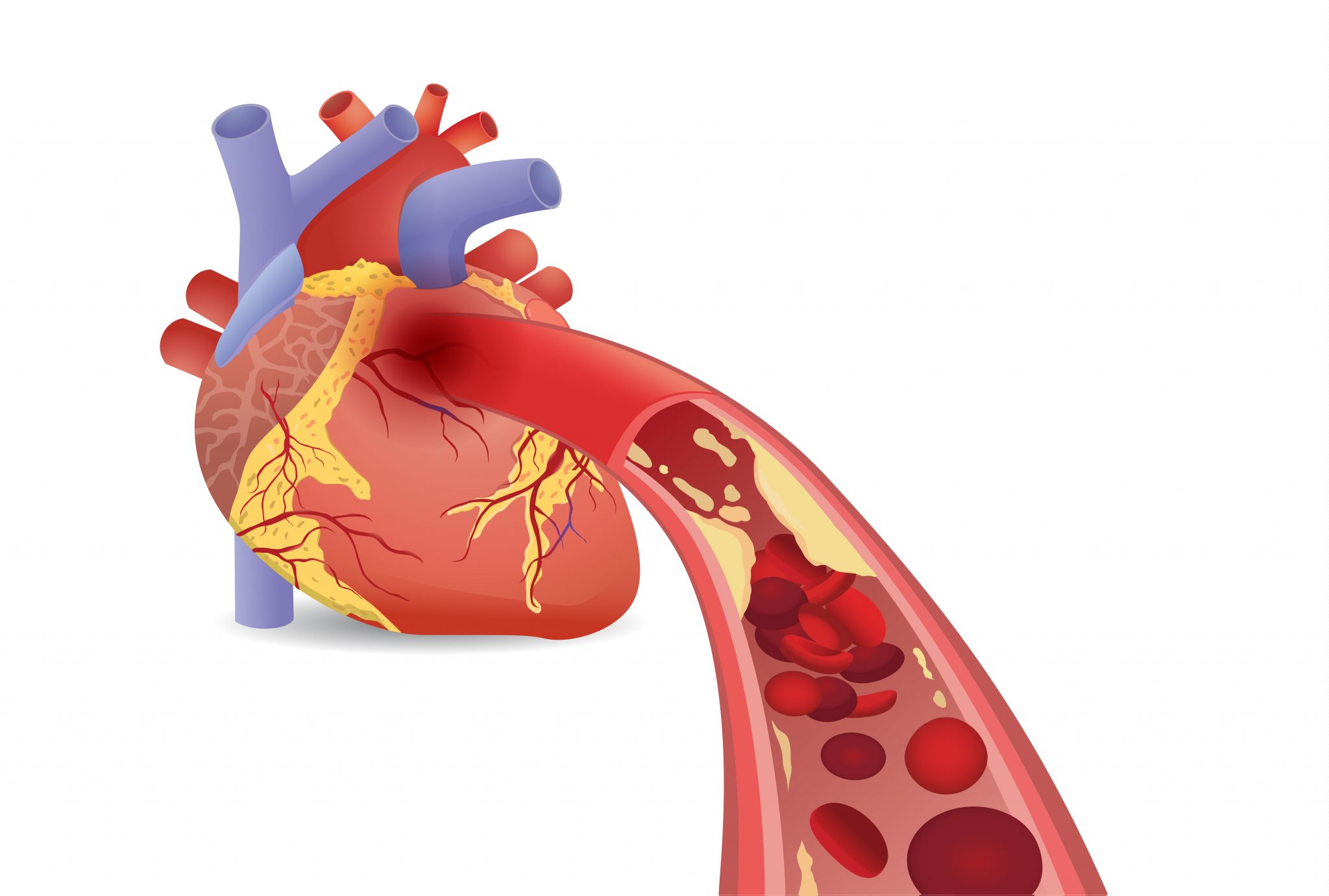
Atherosclerosis
Atherosclerosis is a condition in which the heart’s arteries build up with fatty plaque, composed of fatty substances, cholesterol and cellular waste. The plaque congeals and hardens, forming calcium deposits along the artery walls. The arteries will narrow because of the build-up, restricting blood flow. This condition is also known as coronary artery disease.
Other Conditions Caused by Atherosclerosis
When the blood flow to the heart is restricted by atherosclerosis, sufferers may experience:
- Chest pains
- Shortness of breath
- Blood clots – Arteries can become so damaged that they rupture, causing blood clots to form. These clots can completely stop blood flow.
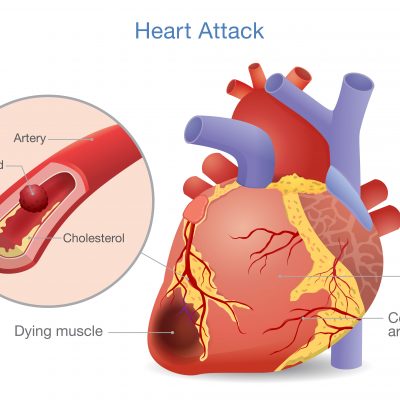
- Heart attack – If a blood clot occurs in an artery that brings blood to the heart, all blood flow will cease, resulting in a heart attack.
- Stroke – If a blood clot occurs in an artery that brings blood to the brain, blood flow will cease, resulting in a stroke.
- Gangrene – If a blood clot occurs in an artery that brings blood to an extremity, such as an arm or leg, the blood flow to the limb will cease. The limb will get gangrene, a condition where the tissue decays. Usually gangrene results in amputation of the affected limb.
- Embolization – If part of the plaque detaches and blocks the artery, the person can suffer from a heart attack or stroke, depending on which artery is blocked.
Prevention
People who are diabetic, drink heavily, have high blood pressure, have high cholesterol, eat a high-fat diet, are obese, who smoke or who have a family history of heart disease are at higher risk for developing atherosclerosis. For anyone to prevent atherosclerosis, patients are advised to:
- Eat a well-balanced diet. Avoid eating fatty foods, and eat meals low in fat and cholesterol.
- Decrease alcohol intake to no more than one or two drinks per day.
- Start and maintain an exercise routine. If you are not overweight, exercising for 30 minutes a day is sufficient. If you are overweight, exercise for 60 – 90 minutes a day.
- Keep your blood pressure below 140/90 mmHg, and have it checked once or twice a year.
- Have your cholesterol checked at least once a year. If it is high, ask your doctor about changing your diet or starting a medication.
Cardiac Condition Treatments
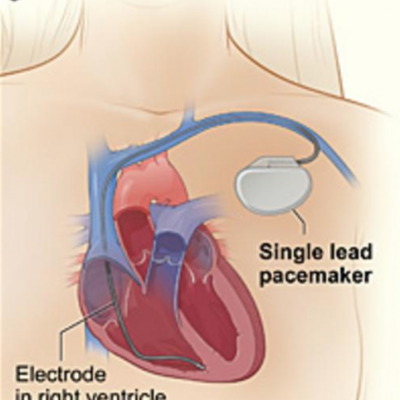
Cardiac Pacemaker
A pacemaker is a small device that is placed in the chest under the skin near your heart to help control abnormal heart rhythms. There are a wide range of causes for heartbeat disruptions and arrhythmias, but, regardless of the underlying cause of the abnormal heart rate a patient is experiencing, a pacemaker may fix it.
A pacemaker can be implanted in your chest with a minor surgery. The surgery takes only a few hours, but you will remain in the hospital overnight, so your heartbeat can be monitored and your cardiologist can make sure that your pacemaker is working correctly. Most people return to their normal activities within a few days of having their cardiac pacemaker installed. Avoid vigorous exercise and heavy lifting right after your surgery and until you are cleared by your doctor. Your doctor can determine what level of activity is appropriate for you post-surgery.
A pacemaker is made up of a battery, a computerized generation system and wires with sensors called electrodes. Pacemaker batteries usually last between 5 and 15 years, depending on how much your pacemaker is activated. Electrodes monitor your heart’s electrical activity and send the information through the wires to the computer generator. Using low-energy electrical pulses your pacemaker keeps the heartbeat at a normal rate. If your heart rhythm becomes abnormal, the computer will direct the generator to send electrical pulses through the wires to your heart, so that its rhythm returns to normal.
We always advise that you inform all of your doctors, dentists and other medical care providers that you have a pacemaker.
Coronary Artery Disease
Coronary artery disease occurs when the coronary arteries become diseased or damaged due to the accumulation of plaques in the arteries (Atherosclerosis). The coronary arteries are the main vessels that provide blood, oxygen and nutrients to the heart. Plaques are fatty deposits consisting of cholesterol and other cellular waste products. Build up of plaques narrow the coronary arteries, causing the heart to receive less blood.
Coronary artery disease can lead to heart attacks, heart failure and an abnormal heart rhythm (arrhythmia).
Coronary artery disease typically develops overtime, and can go unnoticed until a heart attack strikes. Symptoms of coronary artery disease include:
- Shortness of breath – If the heart cannot pump an adequate amount of blood to meet the needs of your body, you may experience shortness of breath or extreme exhaustion following physical exertion.
- Angina (chest pain) – Angina is a feeling of tightness or pressure in the chest. For some people, specifically women, angina may present itself as a sharp or brief pain in the back, arm or abdomen.
- Heart attack – If the coronary arteries are completely blocked, a heart attack may occur. You’re having a heart attack if you experience a crushing pressure in your chest, and pain in your arm or shoulder, sometimes accompanied by sweating and shortness of breath. In some cases, a heart attack can occur without any warning signs.
Risk Factors
The following factors put you at a higher risk for developing coronary artery disease:
- A family history of heart disease, especially if a close family member (father, brother, mother or sister) was diagnosed at an early age.
- Age – Getting older increases the possibility of damaged and narrowed arteries.
- Gender – Typically, men are much more likely to develop coronary artery disease. But, the risk for women increases following menopause.
- Smoking – Nicotine narrows blood vessels. Carbon monoxide can damage the inner lining of blood vessels, making them more prone to atherosclerosis.
- High Blood Pressure – High blood pressure that is not managed can cause the arteries to harden and thicken, thus narrowing the channel through which blood flows.
- High Blood Cholesterol levels can increase the likelihood of plaques and atherosclerosis.
- Diabetes, obesity, lack of exercise and high stress can also out you at a higher risk for developing coronary artery disease.

Treatment
Treatment for coronary artery disease consists of lifestyle changes, as well as drugs and medical procedures, if necessary.
Prevention
- Lifestyle changes can also prevent or slow the advancement of coronary artery disease.
- These changes include exercising regularly, maintaining a healthy diet and weight, and finding ways to reduce stress.
- If you’re a smoker, kicking the habit is also a necessary lifestyle change.
See Your Doctor
- In addition to lifestyle changes, be sure to regularly see your physician, especially if you have been diagnosed with diabetes, high blood pressure or high cholesterol.
- All these solutions can put you on the road to better heart health for a lifetime.
Hypertension
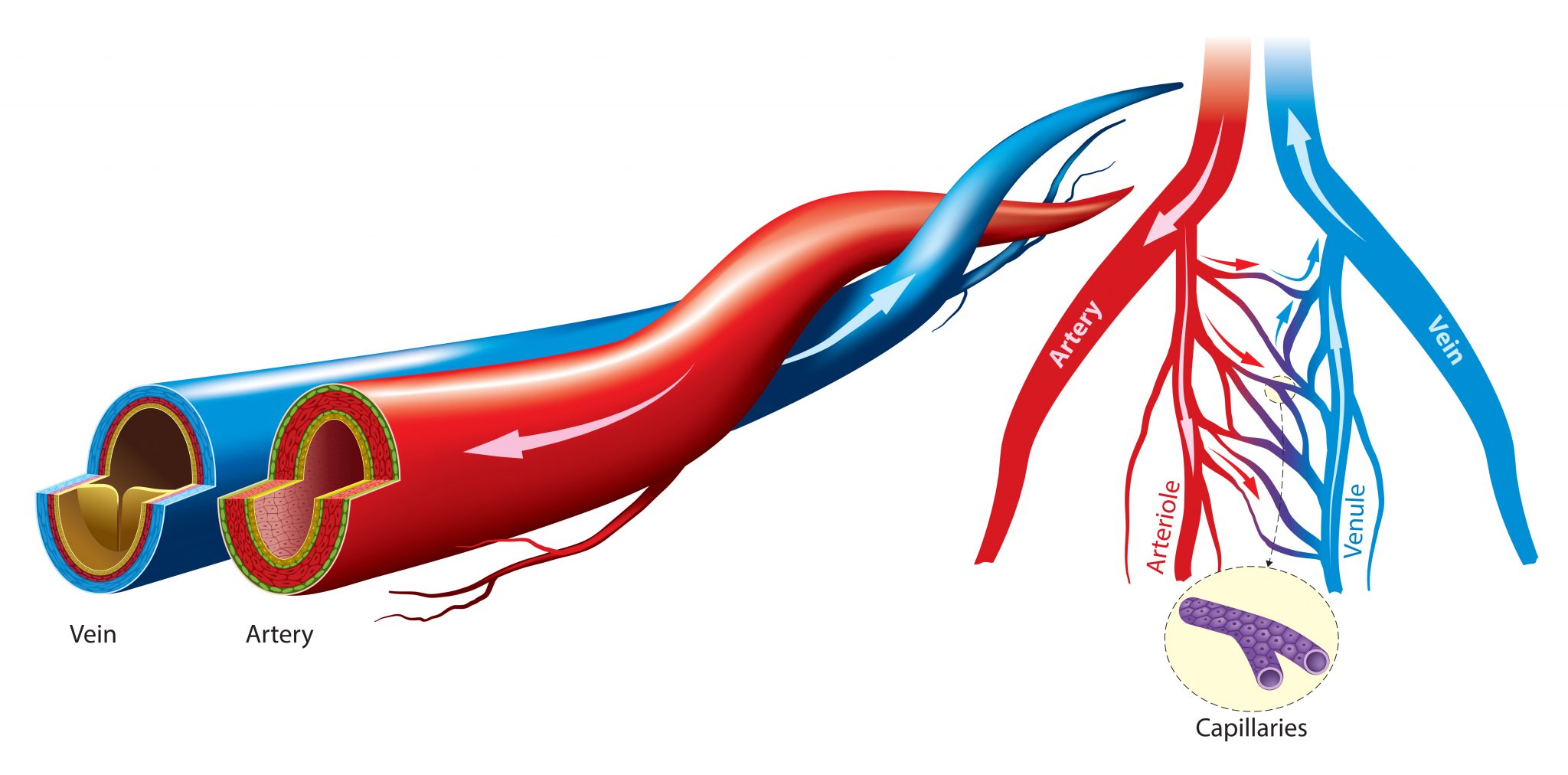
Blood pressure is the force applied to the interior walls of arteries and blood vessels by the flow of blood. This pressure is comparative to the elasticity and size of the artery or blood vessel and relative to the strength of the heartbeat.
Blood pressure is measured in millimeters of mercury (mmHg), and a reading is given in fraction form with two numbers: a systolic pressure number and a diastolic pressure number. The systolic pressure number is on top, which indicates the pressure created in your arteries or blood vessels when your heart beats. The diastolic pressure number is on bottom and indicates the pressure in your arteries or blood vessels when your heart is at rest in between each beat. For an adult, a normal blood pressure should be below 140/90 mmHg. If one or both of these numbers is too high, this is known as hypertension, or high blood pressure.

Causes of Hypertension
Your hypertension can occur on its own without an identifiable cause. This is the most common type and is referred to as essential hypertension. If you experience hypertension as a result of another condition, your diet, a habit or a medication, you have secondary hypertension. Factors that can cause secondary hypertension include:
- Water and salt intake
- Alcohol intake
- Obesity
- Pregnancy (known as gestational hypertension)
- Diabetes
- Medications, such as birth control pills, appetite suppressants, cold medications, migraine medications
- Kidney diseases, such as inflammation, kidney failure, renal artery stenosis or renal vascular obstruction

Prevention
People who have a family history of high blood pressure, are diabetic, who smoke or are obese are at higher risk for developing hypertension. It is usually more prevalent in African Americans than Caucasians as well. For anyone to prevent the onset of hypertension, patients are advised to:
- Eat a well-balanced diet. Avoid eating fatty foods, and eat meals low in fat and cholesterol.
- Decrease alcohol intake to no more than one or two drinks per day.
- Stop smoking.
- Start and maintain an exercise routine of at least 30 minutes a day.
- If you are overweight, you are advised to lose the extra weight.
- If you are diabetic, regulate your blood sugar levels.
- Manage or reduce your stress.

Treatment
If you are diagnosed with hypertension, your doctor will likely suggest you follow the prevention guidelines listed above. If these lifestyle changes do not lower your blood pressure, you can also begin taking a medication prescribed by your doctor. Sometimes one medication may not regulate your blood pressure, and you may be prescribed two or more to take together. Please take the medication(s) prescribed to you as directed. If you experience any side effects from your medication(s), please alert your doctor as soon as possible.
Myocardial Infarction
A myocardial infarction, also known as a heart attack, occurs when the flow of blood through a coronary artery is blocked due to a blood clot. The coronary arteries are main blood vessels that supply blood, oxygen and other nutrients to the heart. Obstructed blood flow to the heart can destroy or damage the muscle of the heart.
Common symptoms of a heart attack include:
- Shortness of breath
- Sweating
- Fullness or squeezing pain in the middle of the chest for more than a few minutes
- Fainting
- Vomiting and nausea
- Persistent upper abdominal pain
- Pain in the shoulder, arm, back, teeth or jaw
- Increasing occurrences of chest pain
Women may experience additional symptoms, such as heartburn, pain in the abdomen, clammy skin and dizziness. They may also be unusually fatigued.
Remember, every person who has a heart attack does not have the same symptoms. Moreover, every person does not experience symptoms to the same degree. Some people do not have any symptoms.
A heart attack can occur during activity, at work, and even at rest. While some heart attacks occur suddenly, many persons experience symptoms or warning signs, hours, days or weeks prior to an attack.
If you think you may be having a heart attack, call 911 immediately. Immediate care can prevent or limit damage to the heart.

Risk Factors
High blood pressure, diabetes, smoking and long-term exposure to second-hand smoke can put you at a higher risk for experiencing a heart attack. In addition, if you’re a woman over 55 or a man over 45, you are also more likely to have a heart attack. Other risk factors include a family history of heart attacks, lack of exercise, obesity and too much stress.

Complications
The damage caused by a heart attack can cause abnormal heart rhythms (arrhythmias), a rupture in the heart, and valve problems; all of which can be fatal. Heart failure can also occur following an attack, and may be temporary or chronic. Heart failure can cause fatigue, shortness of breath or swelling of the ankles and feet.

Treatment
Treatment following a heart attack depends on the severity of your condition and the degree of damage to the heart. Your treatment plan may require medications. You may be given Aspirin to decrease blood clotting or thrombolytics to help dissolve a blood clot that is obstructing the flow of blood to your heart. Doctors may also give you drugs to prevent new blood clots from forming, or blood thinners to make your blood less “sticky,” and thus less likely to form more clots. Pain relievers, such as morphine can relieve chest pain. Nitroglycerin may be administered to treat chest pain. It opens arterial blood vessels temporarily to improve blood flow to and from the heart.
Further Treatment
In addition to medications, surgery may also be necessary. Your doctor may perform a coronary angioplasty to open blocked coronary arteries, thus improving blood flow. Along with this procedure, a stent may be inserted to keep the artery open long term to restore blood flow to the heart.
In rare circumstances, at the time of a heart attack, a coronary artery bypass surgery may be performed, During this procedure, veins or arteries are sewed in place at a region beyond the blocked coronary artery, to restore blood flow. Most likely, your doctor may recommend this surgery after your heart has had time to recover from the attack.
Prevention
Promoting a healthy heart must become a way of life. Regular exercise, a healthy diet, annual medical exams, regular cholesterol and blood pressure checks, and stress management can prevent heart attacks or help you recover if you’ve had one. In addition, if you are a smoker, the simplest, most significant thing you can do to improve the health of your heart is to stop. Avoiding exposure to second-hand smoke and drinking alcohol in moderation can also help.
These simple lifestyle changes play an important role in preventing heart attacks.

Cardiac Catheterization
Cardiac catheterization is an invasive procedure performed to identify problems in the heart. During the procedure, using a long thin tube called a catheter, your cardiologist can:
- Identify blockages or narrowing of the blood vessels
- Determine the amount of oxygen in the heart
- Identify problems affecting the valves of the heart
- Identify congenital heart defects
- Take a biopsy (tissue) from the heart
- Test the pressure inside the heart
Some heart disease treatments, such as an angioplasty, are also performed using cardiac catheterization. During an angioplasty, a tiny balloon is inserted temporarily to help widen a narrow artery.
- How do I prepare for the procedure?
- What happens during the procedure?
- What happens after the procedure?
- Results
- Risks
To ensure optimal results, do not eat or drink anything eight to 12 hours before the procedure. Remember to bring all your medications, including supplements with you on the day of your procedure. Lastly, although it’s quite normal for you to feel nervous or anxious about the procedure, try to relax. Nervousness may cause your heart to beat rapidly and irregularly, causing results to be inaccurate.
Cardiac catheterization is performed in a special operating room within a hospital, known as the catheterization lab. This lab contains X-ray and imaging machines that normal operating rooms do not have.
You’ll be awake during the procedure, but sedated, so you’ll be able to follow instructions. The nurse will insert an IV in your arm or hand in case you need additional medications during the procedure. Your heartbeat will also be monitored.
Prior to inserting the catheter in your artery, you’ll receive a shot of anesthetic to numb the area. The catheter may be inserted in an artery or vein in your neck, arm, or groin. The catheter will be threaded through the blood vessels to the heart. You should not feel any pain or feel the catheter moving through your body. If you experience any discomfort, inform your cardiologist.
Typically, it takes several hours to recover. Following the procedure, you’ll be taken to a recovery room, where you’ll remain until the anesthesia wears off, which usually happens within an hour. After recovery, you’ll be placed in a hospital room.
Do not move the limb that your catheter was inserted in to, as this could cause serious bleeding. Once the nurse removes the catheter, he or she will apply pressure to the insertion site. You’ll have to lie flat for one to six hours to prevent severe bleeding and to enable the artery to heal.
You will be given food or drink after the procedure. You may be able to go home the same day or you may have to stay a little longer, depending on your condition, and the extent of your procedure.
The results of a cardiac catheterization may indicate that surgery or another treatment is necessary. Your cardiologist will thoroughly discuss the results and treatment options with you.
As with any procedure performed on the heart and blood vessels, there are some risks. Risks include:
- Bleeding
- Heart attack
- Bruising
- Stroke
- Infection
- Blood clots
- Kidney damage
- Irregular heart rhythm
- Damage to the artery where the catheter was inserted
Major complications as a result of a cardiac catheterization rarely occur.
Remember your cardiologist has recommended this procedure, because the benefits of treating your heart condition far outweigh the risks.

